undefined
undefined
The Syndrome of right bundle
branch block,
ST segment elevation
and sudden death.
By Andrea Nava, Bortolo Martini
If you wish to make comments, to receive further data or to send more details please contact:
bmartini@tiscalinet.it
Padua, March 10, 1999
The first patient with this syndrome was admitted to hospital because of ventricular fibrillation on 24 december 1980 (pt. 4 reported in Am Heart J 1989;118:1203-9)
The second one in 1984 (pt. 3), and the third one in 1995 (pt.1).
The first published image of a pt. (pt 1 of Am Heart J), with VF (and the syndrome) appeared in 1986 in the "New trends in arrhythmias" by Nava A , Scognamiglio R, Buja GF, Daliento L, Bottero M. Canciani B, Corrado D, Stritoni P, Fasoli G, Martini B, Thiene g: Arrhythmogenic right ventricle. Clinical spectrum and familiarity. 1986;2:13-19 (see fig. 5 and 6), but no details were given on the resting ECG.
We also published some incomplete data on the "Giornale Italiano di Cardiologia" in 1986 (pt 11-29 and 30): Nava A, Canciani B, Scognamiglio R, Buja GF, Daliento L, Miraglia G, Martini B, Thiene G. La tachicardia e la fibrillazione ventricolare nel ventricolo destro aritmogeno. G Ital cardiol 1986;16:741-9
In 1988 we published the first detailed written description of syndrome in two abstract in Giornale Italiano di Cardiologia:
1) Nava A, Canciani B, Martini B Buja GF. La ripolarizzazione precoce nelle precordiali destre. Correlazioni ECG-VCG-elettrofisiologia G Ital Cardiol abstract 1988 suppl 1 ;18:118
2) Martini B, Nava A, Buja GF, Canciani B, Thiene G. Fibrillazione ventricolare in apparente assenza di cardiopatia. Descrizione di 6 casi. G Ital Cardiol abstract 1988 suppl 1 ;18:136
In 1988 the first (for what we know) ecg trace of the syndrome was presented in "Mises a Jour Cardiologiques" 1988;XVII,5:157-9
In 1988, the first complete description of the syndrome, was published in the American Heart Journal (19889;118:1203-9
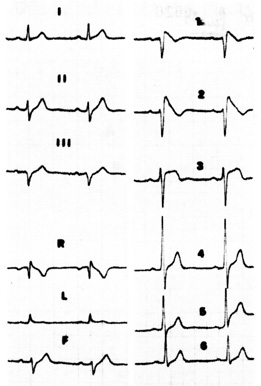
This is the first published ECG trace in Medical literature (MISES A JOUR CARDIOLOGIQUES -17 ANNEE
1988 -XVII, 5, P 157-9), of a pt. resuscitated from sudden cardiac death, and admitted to Hospital in 1984 at the age of 34 years. The pt is still alive under amiodarone therapy. He did have any relapse. (pt. 3 of Am Heart J 1989)
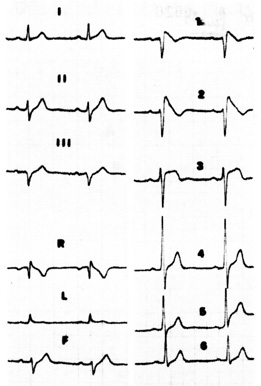
This is the figure published in Am Heart J 1989;118:120-1209 which proposes 6 pts affected by "idiopathic ventricular fibrillation". All the different pattern of the syndrome are documented. Pt 1 had a RBBB + St segment elevation. Pt 3 (the same published in 1987 in the figure at the top) had the so colled J wave. Pt 4 had RBB + ST elevation + LAD + first degree A-V block. In this pt., admitted to hospital because of ventricular fibrillation in 1975 and died suddenly in 1981, necropsy study demonstrated right ventricular cardiomyopathy and extensive sclerosis of the conduction system (see article in J Am Coll Cardiol 1996;27:443-8). Pt 2 and 5 had isolated ST segment elevation.
The syndrome described by our group is characterized by:
a- juvenile aborted sudden death
b- familial involvement
c- male predominance
-ECG patterns of:
1) different degrees of right bundle branch block
2) St segment elevation in V1-V3 (which can be an isolated pattern)
3) sometime left axis deviation
4) prolonged HV interval in the cases with major conduction abnormalities
5) frequent positive late potentials study
d- unrare demonstrable evidence after detailed examination (including necropsy in rare cases) of some concealed organic heart disesease, particularly of the right ventricle.
e- the disease rarely maps (latest data will be presented at NASPE), in the same loci of right ventricular cardiomyopathy.
After Aihiara in 1990, in 1992, the Brugada Brothers published 8 more patients with the same clinical and ECG syndrome, in whom (apart from HV prolongation in 4 pts), they did not evidence any significant heart disease. In 1998 the same group gave evidence of a genetic ion channel disease in some of their pts. (www.brugada.crtia.be/.)
In the following pages we present the abstract of the 3 main articles on the syndrome, and the detailed review article published in 1997 in the book: arrhythmogenic right ventricular cardiomyopathy/dysplasia. A.Nava, L. Rossi G. Thiene editors. Elsevier science BV
A complete bibliography on the syndrome is also presented at the end
LA REPOLARISATION PRECOCE DANS LE PRECORDIALES
DROITES: TROUBLE DE LA CONDUCTION INTRAVENTRICULAIRE
DROITE?
CORRELATIONS DE L'ELECTROCARDIOGRAPHIE-VECTORCARDIO-
GRAPHIE AVEC L'ELECTROPHYSIOLOGIE
A.Nava, B. Canciani, M.L. Schiavinato, B. Martini, G.F. Buja
Dep. de Cardio. Univ. De Padoue (Italie)
MISES A JOUR CARDIOLOGIQUES -17 ANNEE 1988 -XVII, 5, P 157-9
_____________________________________________________________________________________________________________________
MATERIEL E METHODES
Il s'agit de 6 sujets (4 hommes et 2 femmes) àgés de 26 a 30 ans.
L'ECG montrait un sus déclage de ST (1-4 mm) supérieur a 2 mm de V1 a V5 ou de V1 a V4.....
Chez 5 de ces sujets le diagniose de dysplasie du ventricule dorit a pu etre posé. Le sixième n'avait pas de cardiopathie mais il avait présenté un épisode de fibrillation ventriculaire. Une exploration électrophysiologique s'est imposée dans 3 cas: 2 fois à cause d'un episode de FV; le troiseè sujet etait un jeune asymptomatique dont le frère était décédé subitement......
A l'ètude electrphysiologique, on remarque au niveau du septum moyen-haut, un QRS allongé qui va de 120 à 150 msec et la dernière portion (40-50 msec) coincidait avec la partie initiale et moyenne de la ripolarisation.....
Le susdécalage de ST etait secondaire non pas à une repolarisation précoce mais du moins en partie à une dépolarisation retardée.
____________________________________________________
Ventricular fibrillation without apparent heart
disease: Description of six cases
Since 1977, six patients (five males and one female), aged 14 to 35 years, resuscitated from
Ventricular fibrillation, were referred to our department for detailed evaluation, after exclusion of
major cardiac pathologic conditions. Four patients had a family history of heart disease. Basic
ECGs showed sinus rhythm in all of them. PR interval was prolonged in one. Two patients had
complete and one had incomplete right bundle branch block. One patient had inverted t waves in V1-V3 and late potentials. Three had an upslooping ST_T segment elevation in V1-V2. The
cardiothoracic index was less than 0.5 in five and 0.50 in one. In one of the five patients studied,
the clinical episodes of ventricular fibrillation was reproduced by stimulation of the right
ventricular outflow tract during electrophysiologic study. Results of cross-sectional
echocardiography and angiography showed predominantly structural and wal motion
abnormalities of the right ventricle in five patients and slight wall motion abnormalities of the left
ventricle in two. Two pwo patients had also mitral and tricuspid valve prolapse. Coronary arteries
were normal in all five patients examined. Results of endomyocardial biopsy showed no
abnormalities in one patient, fibrosis in two, and fibrolipomatosis in one. Two patients died
during follow-up: autopsy was performed in one and results showed right ventricular
cardiomyopathy. Thus in five of these selected patients with apparently idiopathic ventricular
fibrillation, some abnormalities, predominantly of the right ventricle, were documented only after
detailed investigation; however, clinical history and some nonspecific ECG abnormalities were factors in the diagnostic procedure. (Am Heart J 1989;118;6:1203.)
Bortolo Martini, MD, Andrea Nava, MD, Gaetano Thiene, MD,
Gian Franco Buja, MD, Bruno Canciani, MD, Roldano Scognamiglio, MD,
Luciano Daliento, MD, Sergio Dalla Volta, MD. Padua, Italy
________________________________________________________________________________________________________
Familial Cardiomyopathy Underlies Syndrome of Right Bundle Branch Block, ST Segment Elevation and Sudden Death
DOMENICO CORRADO, MD, ANDREA NAVA, MD, GIANFRANCO BUJA,MD,
BORTOLO MARTINI, MD, GIUSEPPE FASOLI, MD, LUCA OSELLADORE, MD,
PIETRO TURRINI, MD, GAETANO THIENE, FESC
Padua, Italy
______________________________________________________________________________
Objectives. We sought to assess wether structural heart disease underlies the syndrome of right bundle branch block, per- sistent ST segment elevation and sudden death.
Background. Ventricular fibrillation and sudden death may occur in patients with a distinctive electrocardiographic (ECG) pattern of right bundle branch block and persistent ST segment elevation in the right precordial leads.
Methods. Sixteen membres of a family affected by this syndrome underwent noninvasive cardiac evaluation, including electrocardiography, Holter ambulatory ECG monitoring, stress testing, echocardiography and signal-averaged electrocardiography; two patients had electrophysiologic and angiographic study. Endomyocardial biopsy was performed in one living patient, and postmortem examination, including study of the specialized conduction system, was performed in one victim of sudden death.
Results. Five years before a fatal cardia arrest, the proband had been resuscitated from sudden cardiac arrest due to recorded ventricular fibrillation. Serial ECGs showed a a prolonged PR interval, right bundle branch block, left axis deviation and persistent ST segment elevation in the right precordial leads, in the absence of clinical heart disease. Postmortem investigation disclosed right ventricular dilation and myocardial atrophy with adipose replacement of the right ventricular free wall as well as sclerotic interruption of the right bundle branch. A variable degree of right bundle branch block and upslooping right precordial ST segment was observed in seven family members; four of the seven had structural right ventriccular right ventricular abnormalities on echocardiography and late potentials on the signal-averaged electrocardiography. A sib of the proband also had a prolonged HV interval, inducible ventriculat tachycardia and fibrofatty replacement on endomyocardia byopsy.
Conclusions. An autosominal dominant familial cardiomyopathy, mainly involving the right ventricle and the conduction system, accounted for the ECG changes and the electrical instability of the syndrome.
(I Am Coll Cardiol 1996;27:443-8)
_____________________________________________________________________________________________________________________
Syndrome of right bundle branch block, ST segment elevation
and sudden death: evidence of an organic substrate
Bortolo Martini M.D, Domenico Corrado, Andrea Nava and Gaetano Thiene
1997 Elsevier Science B.V.
In: Arrhytmogenic right ventricular cardiomyopathy/dysplasia
A.Nava, L.Rossi, G.Thiene Editors
Abstract:
Non-ischemic upslooping ST segment elevation in the precordial leads has been recognised for decades in electrocardiography. Early reports ascribed this pattern to a normal variant, which was called "early repolarisation syndrome". This electrocardiographic (ECG) feature was usually described as an isolated pattern, without any coexistent conduction or myocardial abnormalities. A similar ECG pattern was observed in patients with severe hypothermia and different acute pathologic conditions.
In 1989 the group from Padua described an association between early repolarization, right bundle branch block (RBBB) of different degree, juvenile sudden death and right ventricular abnormalities, possible consistent with minor localised forms of right ventricular dysplasia/ cardiomyopathy [1]. Since then, a number of reports (summarized in table 1), have been published regarding this rare electrocardiographic (ECG) pattern and its clinical and diagnostic associations [1-20].
Despite identical or similar ECG patterns of the syndrome, two different pathogenesis are proposed. The first one, associates the RBBB+ST elevation with some organic ( and sometime genetically transmitted) heart disease of the right ventricle; the ECG pattern is linked to localized areas (septal and parietal) of the right ventricle in which there is a slowing and dispersion of depolarization. The second one ascribes the same electrocardiographic and clinical pattern to a different entity, namely an unknown idiopathic and functional electrical abnormality of some myocardial tissue (perhaps the M cells), producing dispersion of refractoriness and extreme anysotropic conduction. The purpose of this study is to examine the published cases of the disease, and to discuss the different pathogenesis proposed.
Definition of the term of "early repolarization"
In the absence of ischaemia, pericarditis, electrolytic abnormalities, long QT syndrome, "idiopathic " ST segment elevation has been longly recognized in clinical electrocardiography, since the initial description of Shipley et al. [21], on a four lead electrocardiogram. The most common pattern of this elevation with upward concavity has been named early repolarisation. The elevation, coincides with the the point on the ECG at which there is abrupt transition from the QRS complex to the ST segment (J point). It is usually recorded in the left precordial leads alone or simultaneously in the inferior leads; ST elevation restricted to the right precordial leads is unusual, according to the experience of Parisi et al. [22], who examined 49512 healthy males tracing.
According to Kambara, Wassemburg et al. [23,24] "early repolarization" include RS-T segment elevation of a minimum of 0.5 mm above baseline (greater than 2 mm in exceptional cases) in at least 2 limbs or precordial leads. Early repolarisation occurs in approximately 2.5% of adults and appear to be most commonly encountered in young black males. A similar electrocardiographic pattern is observed in the so called "vagotonia". RS-T elevation, which can be transient, may often persists for decades in many patients, and usually decreases with advancing age.
Intraventricular conduction disturbance namely right or left bundle branch block have been never proposed as a part of this entity, but minor QRS and T waves changes have been sometime described in early repolarization.
These QRS changes often associated to early repolarization, are characterized by nothching in the terminal portion of QRS at the J point, called J wave. Like early repolarization, the J wave is typically encountered in V3-V6 and in the inferior leads; sometime it is not a distinct wave but a slurred downstroke of the QRS complex (late delta wave).
In the recent literature the term J wave includes both the terminal QRS nothching and/or early repolarization [25 ]. As discussed before, however, early repolarization or J wave which is rarely seen in leads V1-V2 [21] should better named atypical J wave.
Atypical J wave is similar but distinct from incomplete RBBB as the terminal vector is not directed to the right but anteriorly and slightly leftward in the orizontal plane. In the ECG trace of these pts there is not a small slurred terminal vector in V6 and aVR, as it is expected in incomplete RBB. For these reasons, typical and atypical J wave are not the same electrocardiographic entity also if it has been recently hypothised that they might have the same electrogenesis but a different origin, namely typical J wave from the left ventricle and atypical J wave (R') from the right ventricle [26].
The T waves can be tall and peaked in early repolarisation; T wave inversion can be present as an unusual finding.
Typically RS-T changes normalise following isoproterenol infusion [27], increase following propanolol, and do not change after atropine.
The physiologic basis for early repolarization or J wave was considered the result of early onset of ventricular repolarization in a non-homogeneous manner which causes a difference of potential between myocardial areas resulting in ST elevation.The anomalous gradient between a site with faster recovery, underlying the exploring lead, and a site with slower recovery could be related to enhanced activity of the right sympathetic nerves which can be normalised by beta adrenergic stimulation [27].
Historical notes and pathophysiology of early repolarization associated to diseases
The J wave was firstly published in 1938 by Tomaszewski et al. [28] obtained in a man exposed to severe hypothermia. Osborn et al. [29] observed that all but one the hypothermic animals that developed ventricular fibrillation had J waves. J wave (particularly the atypical pattern), was further observed in patient with subarachnoid haemorrhage, brain injury, brain death, right radical neck surgery with destruction of sympathetic nerve fibres, and during resuscitation from cardiac arrest [10,25].
The recent elegant experimental observations of Yan and Antzelevitch [26] have tried to clarify part of this problem. They started from the old clinical observations that in severely hypothermic or hypercalcemic mammalians the ECG is characterized by J deflection. In animals the J wave is commonly observed under baseline conditions and is greatly amplified under hypothermic conditions. This author demonstrated in a canine model, that heterogeneous distribution of an Ito-mediated spike-and dome morphology of the action potential across the ventricular wall underlies the manifestation of the electrocardiographic J wave. A prominent Ito is the responsible for the relatively large phase 1 and the characteristic spike-and-dome configuration of the epicardial action potential. The absence of prominent notch in the endocardial action potential is correlated with a much smaller Ito. Cells in the M region may contribute to the J wave. The presence of a prominent potential notch in the epicardium but not endocardium is shown to provide a voltage gradient that manifest as a J wave or elevated J point at the R-ST junction of the ECG.
Antzelevich has demonstrated a highly significant correlation between the amplitude of the epicardial action potential notch and that of the J wave recorded during intervention that alter the appearance of the electrocardiographic J wave, including hypothermia, premature stimulation, and block of Ito by 4 aminopyridine. Ventricular activation from endocardium to epicardium, with epicardium activated last, was a prerequisite for the appearance of the J wave. This sequence permits the establishment of a voltage gradient of the early phases of the action potential after activation (i.e., the QRS) is complete.
The spike-and dome morphology of the right ventricular action potentials are more accentuated than that of the left ventricular epicardium. Despite the larger notch, because of the thinner ventricular wall and a briefer activation time, the right ventricular epicardial action potential notch occurs during the QRS and is obscured. This explain why the J wave is manifested (in animal models) in leads which mainly explore the left ventricle.
The presence of a prominent J wave has been shown to predispose canine ventricular epicardium to all-or-none repolarization and phase 2 re-entry. Under pathologic (not functional) conditions the action potentials plateau (dome) is abolished at some epicardial sites (especially of the right ventricle), causing a marked dispersion of repolarization. Loss of the plateau in epicardium but not endocardium causes elevation of the ST segment or early repolarization syndrome. The appearance of ST-segment elevation only in the right precordial leads is consistent with a loss of the action potential in right but not left ventricular epicardium. Loss of the dome can be accentuated by vagal manoeuvres or class 1 antiarrhythmic drugs, whereas b-adenergic agonist can restore the dome. Propagation of the the action potentials dome from sites at which it is maintained to sites where is abolished can cause local reexcitation (phase 2 re-entry), and produce ventricular arrhythmias.
Definition of the syndrome of aborted sudden death, right bundle branch bloch and early repolarization
This syndrome was described in detail in 1989 from the group in Padua [1], but became popular after the paper by Brugada and Brugada [3] who claimed in 1992 the originality of their "distinct" (not first) observation. In the following years, the published papers on this subjects, insisted sometime on the concept of two "identical but different" syndromes, the one described in Padua associated with an organic heart disease [1,5,7,9,11,14,15,19,20], and the second one associated with a functional disorder [2-4,6,8,10,12,13,16-18]. Marcus [30] and Sheinman [31], have recently expressed the opinion that a clear distinction between the two syndromes is difficult to prove.
There are some typical features of the syndrome, according to our experience and to the literature:
-A familial history of sudden death or similar ECG patterns in members of the same family are not unusual. An autosomal dominant inheritance with different expression seems to be involved [15].
-Aborted sudden death is often the first symptoms, but syncope is not so rare in the clinical history. Few patients (pts) up to now, have been recognized as having an asymptomatic form of the syndrome, and some had a late major clinical event [5,15,17,18].
-The syndrome is usually identified in the second and third decade, but infant and aged cases have been described [3-5,15]. The patients do not shows any cardiac impairment: cardiomegaly is not present and no previous illness possible leading to a cardiac disease were reported. Premature ventricular contractions, sometime polymorphic, are not routinely seen at Holter monitoring.
-Aborted sudden death do not significantly occurs during effort or stressfull situations. Only in occasional cases, a parasympathetic or sympathetic imbalance was proposed [8,10,16]
-The ECG patterns in different patients are similar and include an ST elevation usually associated with some right ventricular conduction disturbance, namely a complete or incomplete RBBB, or an atypical J wave (see before). The degree of RBBB and of ST elevation varies in selected cases over the time, and may be enhanced by pharmacological interventions [17]. R-ST elevation has howeverer been reported to be prominent only in few observations before and after the episode of aborted sudden death [11].
According to epidemiological data, the RBBB-ST pattern is a rare abnormality in asymptomatic pts, with an incidence of 0.63% in 10420 adults over 35 years [32]. In cardiac pts, it may be occasionally seen in pts with anteroseptal myocardial infarction, particularly when high precordial leads are recorded [14].
It has been proposed that also cases with an isolated ST segment elevation and malignant ventricular arrhythmias belongs to the syndrome [11,19,20]. In these cases, pharmacological interventions [17] or the recording of high precordial leads may show the typical pattern [14 ].
-Late potentials study can be positive.
-The electrical abnormality at the time of the resuscitation is ventricular fibrillation (VF); but polymorphic ventricular tachycardia can often be the preceeding ECG event [2,6,10,14]. Occasionally a monomorphic ventricular tachycardia of left bundle branch block morphology has been observed [16,19]. During further investigations, the pts have no spontaneous ventricular arrhythmias apart from isolated and non sustained premature ventricular contractions. During electrophysiologic study, a polymorphic ventricular tachycardia and or a VF is usually inducible. HV interval can be prolonged, usually in the pts with RBBB sometime associated with left axis deviation and prolonged PR interval [1,3,15,16]. A late QRS depolarization has been recorded at the outflow tract of the right ventricle in temporal relation with the ST segment elevation [33].
-Antiarrhythmic therapy is mandatory in these patients. Amiodaron and beta Blockers have been mostly used, but have been unsuccessful in some cases. An implantable defibrillator is becoming the first-choiche therapy with good results [2,4,10,16,17]
Pathogenesis:
In our first case affected by the syndrome and submitted to detailed necropsy, right ventricular dysplasia /cardiomyopathy has been documented [1,15]. Additional preliminary necropsy reports on similar cases have been recently presented [20].
This pt (n° 3 of figure 1), had the first episode of ventricular fibrillation at the age of 24 years. His ECG showed firsts degree A-V block, left axis deviation, incomplete right bundle branch block, ST segmente elevation in the precordial leads (in a later trace, an increased ST elevation and inverted T waves were present in V1-V3 [15]). He had an HV interval of 70 msec. He died 5 years later, of a new episode of ventricular fibrillation. The heart weight was 350 gm; the left ventrice and the coronary arteries were normal. The right ventricle was enlarged (with preserved wall thickness), with marked dilatation of the pulmonary infundibulum; interstitial fibrosis and remarkable myocardial atrophy with transmural fatty replacement replacement of the free wall, the infundibulum and the moderator band. Results of histologic examination of the specialized atrioventricular junction showed remarkable fibrosis of the bifurcating bundle and proximal bundle branches. Considering the ECG disturbance, the prolonged HV interval, and the pathological results, we [15] suggested the presence of a double ventricular conduction defect, one in the septal area (responsible for the prolonged HV interval), and a second one at a localized right parietal site. This second delay, previously documented in similar patients affected by right ventricular dysplasia/cardiomyopathy, by epicardial mapping [34], can be further demonstrated by late potentials studies and by the direct recording during intracavitary study, of right ventricular depolarization electrical activity at the time of the abnormal ST segment [15,33,35]. This marked dispersion of ventricular activation times is likely to predispose to ventricular arrhythmias.
Apart from this necropsy evidence of a cardiac disease, more patients with the syndrome have been identified as having some concealed structural heart abnormality, particularly of the right ventricle [1,5,7,9,11,14,15,19,20]. The proposed diagnosis derived from 2D echo, angiography, bioptic studies, of both the left and right heart. Further data has come from the family study, the signal-averaged-ECG and the electrophysiologic recordings, the magnetic resonance imaging; in the near future the genetic analysis is expected to provide further informations.
The "distinct" syndrome later proposed lately [3] does much differ from our original description, apart from the absence of any cardiac disease in Brugada's patients, according to His investigational results. The number of patients with this "distinct" disorder, subsequently published, is not well definited because it is not clear if some of the patients described in Their registry [17] have also been described in other papers [2-4,6,8,10,12,13,16-18].
Brugada, while identifying a functional disorder, has lacked details regarding echocardiography, late potentials study, angiography, biopsy, magnetic resonance imaging, and necropsy examination in the 6 pts who died suddenly [3,17]. He could particularly not explain, why four of the eight patients in the first serie had a prolonged HV interval, which strongly suggested a structural disease at least of the His-Purkinje system.
The hypothesis that a functional cardiac electric disorder can lead to a devastating clinical event like sudden death, is supported in His opinion by:
-the conduction disturbance varies over the time in some patients, going from a absent to an increased degree of the right bundle branch block and ST segment elevation. On this base Brugada has also hypothised that in some patients affected by "idiopathic" ventricular fibrillation and with a normal recorded electrocardiogram, a concealed form of this disease may occur [17]. Some Asian authors have seen in this hypothesis a possible explanation for some cases of "nocturnal sudden death", with apparently normal ECG [11].
-Different pharmacological and pacing interventions can modify the electrocardiographic pattern.
Bjerregard et al. [10] noticed an enhancement of the wave during faster rates, suggesting a role for the autonomic nervous system. Recently Mijazaki et al. [16] in 4 pts with atypical J wave, noticed that ST segment elevation was augmented by stimulation of alpha-adrenoceptors or muscarinic receptors or by class 1A drugs, but was mitigated by beta-adrenoceptor stimulation or alpha-adrenoceptor blockade. MIBG imaging was negative in these pts. This drove to exclude a significant role for the autonomic system apart from an important modulation activity.
Ajmaline and procainamide can reproduce the typical ECG pattern in patients with a transient or concealed form of the electrical abnormality [17].
-The polymorphic characteristic of the ventricular arrhythmias and their fast cycle length suggest functional re-entry rather than a single re-entrant loop with a changing exit point. The re-entry can be easily triggered by spontaneous or induced premature beats. The underlying pathophysiology abnormality proposed by Brugada [3] was either marked dispersion of refractoriness of cardiac tissue or extreme anisotropic conduction properties of the conduction system and the ventricular muscle. Recently Brugada has speculated the role of a functional abnormality of the M cells in this disease, which could cause an abnormal depolarization- repolarization [17].
Conclusion
In our opinion [1,15,20], supported by others [5,7,9,11,14,15,19,30,31], the syndrome of sudden death, RBBB and ST segment elevation recognises a pathological structural basis in the right ventricle, possibly consistent with a localized form of right ventricular cardiomyopathy.
From the ECG point of view, three pattern can be recognised: 1) Typical complete or incomplete RBBB + ST elevation; 2) Atypical J wave in the precordial leads; 3) Isolated ST elevation in the precordial leads. The clinical and investigational data are similar in the 3 groups.
Right ventricular dysplasia/cardiomyopathy [36,37] is often an autosomic dominant ereditary condition [38], characterised by atrophy and fibro-adipose substituion of the right and less of the left ventricle. Its pathologic and clinical presentation is extremely polymorphic, going from extremely severe involvement of the right and of sometime the left ventricle, to asymptomatic structural abnormalities very difficult to adcertain, but sharing a common problem: a high prevalence of different ventricular arrhythmias and sometime sudden death [36-38]. The disease was always existed, but only after the work of Marcus and Fontaine [36], it was worldwide (sooner or later) recognised. After that report, cases of sudden death and many ventricular arrhythmias, previously retained idiopathic and functional, have recognized their origin from some right ventricular pathology [39-42], always followed by intensive debate and sceticism.
These evidences of a pathologic substrate for idiopathic sudden death and for idiopathic arrhythmias, derived from a careful analysis of old and often forgotten clinical clues like family history, detailed examination of the ECG tracing particularly of the pseudo-normal patterns, accurate analysis and description of the results of invasive and non invasive investigations, correct utylisation of the results of the experimental works, continuous debate and self-criticism. The valorisation of minor abnormalities, was a prerequisite for such analysis, and the researcher's mind was not obscured by what was commonly retained the only true medical knowledege.
The utylisation of these criteria has led to the identification of the syndrome of RBB+ST segment elevation characterised by structural and electrical herat abnormalities. This is perhaps only a little contribution to the prevention of some cases of sudden death but we, and all the scientists who gave some contribution to the syndrome in different countries, expect that the patho-electrogenetic hypothesis, and the diagnostic and therapeutic approach described in this article will further ameliorate.
REFERENCES
- -Martini B, Nava A, Thiene G, Buja G.F., Canciani B, Scognamiglio R, Daliento L, Dalla Volta S. Ventricular fibrillattion without apparent heart disease: description of six case. Am H J 1989;118;6:1203-9
- -Aihara N, Ohe T, Kamakura S., Matsuhisa M., Takagi H., Shimomura K. Clinical and electrophysiologic characteristics of idiopathic ventricular fibrillation. Shinzo 1990;22 (suppl 2).80
- -Brugada P, Brugada J: Right bundle branch block, persistent ST segment elevation and sudden death: a distinct clinical and electrocardiographic syndrome. J Am Coll Cardiol 1992;20:1391-6
- -Proclemer A, Facchin D, Feruglio G, Nucifora R: Fibrillazione ventricolare recidivante, blocco di branca destra, persistente sopraslivellamento del tratto ST in V1-V3: una nuova sindrome aritmica? Descrizione di un caso clinico. G Ital Cardiol 1993;23:1218
- -Naccarella F, Bracchetti D. Aritmie ventricolari maligne ed arresto cardiaco in pazienti con blocco di branca destra, persistente sopraslivellamento del tratto ST T in V1 V3. Probabilmente un quadro di cardiomiopatia aritmogena dell ventricolo destro?. G Ital Cardiol 1993;23:1219-22
- -Miyanuma H, Sakurai M, Odaka H, Yamazaki T., Mitobe H., Muraguti I, Iwama N. Two cases of idiopathic ventricular fibrillation with interesting electrocardiographic findings. Kokyu to Junkan 1993;41:287-91
- -Sumiyoshi M, Nakata Y, Hisaoka T, Ogura S, Nakazato Y, Kawai S, Okada R, Yamaguchi H. A case of idiopathic ventricular fibrillation with incomplete right bundle branch block and persistent ST segment elevation. Jpn Heart J 1993;34:661-6
- -Aizawa Y, Tamura M, Chinushi M, Naitoh N, Uchiyama H, Kusano Y, Hosono H, Shibata A. Idiopathic ventricular fibrillation and bradycardia-dependent intraventricular block. Am Heart J 1993;126:1473-4
- -Wiesfeld AC, Crijns GM, Van Dijk RB et al. Potential role of endomyocardial biopsy in the clinical characterization of patients with idiopathic ventricular fibrillation: Arrhythmogenic right ventricular dysplasia- an undervalued cause. Am Heart J 1994;127;1421-4
- -Bjerregaard P, Gussak I, Kotar S, Gessler JE, Janosik D. Recurrent syncope in a patient with prominent J wave. Am Heart J 1994;127:1426-30
- -Tada H, Aihara N, Ohe T, Yutani C, Shimizu W, Kurita T, Kamakura s, Shimomura K. New insight in idiopathic ventricular fibrillation patients with right precordial ST segment elevation. Circulation 1994;90:1511 (abstract)
- -Ferracci A, Fromer M, Schlapfer J, Pruvot E, Kappemberger L. Fibrillation ventriculaire primitive et recidive precoce; à propos d'un cas associant bloc de branche droit et sus-décalage persistant du segment ST. Arch Mal Coeur 1994;87:1359-1362
- -Nademanee K, Veerakul G, Nimmanit S, Tungsanga K, Chaowakul V, Malasit P. Right bundle branch block and ST segmente elevation, an arrhythmohgenic marker for sudden unexpected death syndrome in young Thai men. Circulation 1995;92:1596 (abstract)
- -Naccarella F, Mezzetti M, Palmieri M, Barbato G, Medda M, Di Niro MR, Cavallari F, Masotti A, Bracchetti D, Nanni G, Rimondini R. Analysis of the ECG pattern "incomplete right bundle branch block and ST elevation in V1 V3 in different clinical subsets. A primary electrical disease or an early high right anteroseptal involvement as in right ventricular dysplasia-cardiomyopathy? Preliminary results. New Trends Arrhythmias 1996;9:405-8
- -Corrado D, Nava A, Buja GF, Martini B, Fasoli G, Oselladore L, Turrini P, Thiene G. Familial cardiomyopathy underlies syndrome of right bundle branch block, ST segment elevation and sudden death. J Am Coll Cardiol 1996;27:443-8
- -MiYazaki T, Mitamura H, Miyoshi S, . Autonomic and antiarrhythmic drug modulation on of the ST segment elevation in patients with Brugada Syndrome. J Am Coll Cardiol 1996;27:1061-70
- -Brugada J, Brugada P. What to do in patients with no structural heart disease and sudden arrhythmic death? Am J Cardiol 1996;78(suppl 5a):69-75
- -Gussak I, Bijerregaard P, Chaitman B. ECG phenomenon called J wave: from hypothermia to Brugada syndrome. European Journal of Cardiac Pacing and Electrophysiology 1996;6:130 (abstract)
- -Sheinman MM. Right bundle branch block and ST Elevation is not a distinct syndrome identifying patients at risk for sudden cardiac death. European Journal of Cardiac Pacing and Electrophysiology 1996;6:7 (abstract)
- -Corrado D, Basso C, Buja GF, Nava A, Thiene G Pathologic substrates of right bundle branch block, persistent right precordial ST segment elevation, and sudden death in young people. EUR J C P E 1996;6:36 (abstract).
- -Shipley RA, Hallaran WR. The four lead electrocardiogram in 200 normal men and women. Am Heart J 1936;325-345
- -Parisi A, Beckman C, Lancaster M. The spectrum of ST segment elevation in the electrocardiogram of healthy adult men. J Electrocardiology 1971;4:137-44
- -Kambara H, Phillips J. Long-term evaluation early repolarization syndrome (normal variant RS-T segment elevation). Am J Cardiol 1976;38:157-61
- -Wassemburg RM, Alt WJ, Lloyd C. The normal RS-T segment elevation variant. Am J Cardiol 1961;8:184-192
- -Gussak I, Bjerregaard P, Egan T, Chaitman B. ECG phenomenon called the J wave. Journal of Electrocardiology. 1995;28:49-58
- -Yan GX, Antzelevitch C. Cellular basis for the electrocardiographic J wave. Circulation 1996;93:372-9
- -Morace G, Padeletti L, Porciani M, Fantini F. Effect of isoproterenol on the "early repolarization " syndrome. Am Heart J 1979;97:343-7
- -Tomaszewski W. Changements electrocardiographiques observes ches un homme mort de froid. Arch Mal Coeur 1938;31:525-8
- -Osborn JJ. Experimental hypothermia: respiratory and blood pH changes in relation to cardiac function. Am J Physiol 1953;175:389-98
- -Marcus FI, Fontaine G. Arrhythmogenic right ventricular dysplasia/cardiomyopathy. PACE 1995;18:1298-1313
- -Sheinman M M. Is the Brugada syndrome a distinct clinical entity? J Cardiovascular Electrophysiology. In press
- -Namiki T, Ogura T, Kuwabara Y, Kobayashi S, Saito T, Masuda Y. Five-year mortality and clinical characteristics of adult subjects with right bundle branch block with ST elevation. Circulation 1995;92:1591 (abstract)
- -Nava A, Canciani B, Schiavinato ML, Martini B, Buja GF. La repolarisation precoce dans le precordiales droites: trouble de la conduction intraventriculaire droite? Correlations de l'electrocardiographie- vectorcardiographie avec l'electro- physiologie. Mises a Jour Cardiologiques 1988;17:157-9
- -Fontaine G, Frank R, Guiraudon G. Signification des troubles de conduction intraventriculaires observés dans la dysplasie aventriculaire droite arytmogene. Arch Mal Coeur 1984;77:872-9
- -Nava A, Canciani B, Buja GF, Martini B, Scognamiglio R, Daliento L, Oselladore L, Thiene G.. El electrocardiograma y el vectorcardiograma en la dysplasia arritmogénica del ventriculo derecho. Revista Latina de Cardiologia 1992;15:276-83
- -Marcus FI, Fontaine GH, Guiraudon G. Right Ventricular Dysplasia: A report of 26 Adult cases. Circulation 1982;65:384-397
- -Thiene G, Nava A, Corrado D, Rossi L, Pennelli N. Right ventricular cardiomyopathy and sudden death in young people. N Engl J Med 1988;318:129-133
- -Nava A, Thiene G, Canciani B, Scognamiglio R, Daliento L, Buja GF, Martini B, Stritoni P, Fasoli G. Familial occurrence of right ventricular dysplasia: a study involving nine families. J Am Coll Cardiol 1988;12:1222-8
- -Nava A, Scognamiglio R, Thiene G, Canciani B, Daliento L, Boffa GM, Stritoni P. A Polymorphic form of familial arrhythmogenic right ventricular dysplasia. Am J Cardiol 1987;59:1405-1409
- -Martini B, Nava A, Thiene G, Buja GF, Miraglia G, Scognamiglio R, Boffa GM, Daliento L. Accelerated idioventricular rhythm of infundibular origin in patients with a concealed form of arrhythmogenic right ventricular dysplasia. Br Heart J 1988;59:564-71
- -Martini B, Nava A, Thiene G, Buja GF, Canciani B, Miraglia G, Scognamiglio R, Daliento L, Dalla Volta S. Monomorphic repetitive rhythms originating from the right ventricular outflow tract in patients with minor forms of right ventricular cardiomyopathy. Intern J Cardiol 1990;27:211-21
- -Corrado D. Thiene G, Nava A, Rossi L., Pennelli N. Sudden death in young competitive athletes: clinico-pathologic correlations in 22 cases. Am J Med 1995;89:588-96
|
-Author
-Year
-N.cases
-[Reference]Angiography (right and left ventricle) or 2D echo or MRI |
|
|
|
|
|
|
|
|
|
|
|
|
|
Martini
1989
3
[1] |
35/M
31/M
24/M |
VF,PVC
VF,PVC
VF,PVC |
yes
yes
yes |
RBBB+ST
J wave+ST+LAD
IRBBB+ST+LAD |
-
Pos
- |
45
45
70 |
NSPVT/VF
PRR
SR |
RVA
RVA
RVA |
Fib
-
Fib Fat |
SD
Asymp
SD
|
Amio.
Amio.
- |
|
Aihara
1990
1
[2] |
25/M |
SPVT/VF,PVC |
? |
IRBBB+ST |
? |
? |
VF |
Negative |
? |
? |
Procainamide |
|
Brugada
1992
8
[3] |
2/M
2/F
46/M
48/M
44/M
53/M
8/F
26/M |
SPVT/VF,PVC
SPVT/VF,PVC
SPVT/VF,PVC
SPVT/VF,PVC
SPVT/VFPVC
SPVT/VF,PVC
SPVT/VF,AF
SPVT/VF,PVC
|
yes
yes
yes
no
no
yes
no
no |
IRBBB+ST
RBBB+ST
RBBB+ST
J wave+ST
J wave+ST
RBBB+ST
J wave+ST
IRBBB+ST |
-
-
-
-
-
-
-
-
|
70
-
80
40
45
65
35
60 |
NSPVT
-
SPVT/VF
SPVT/VF
NSPVT
NSPVT
SPVT/VF
SPVT/VF |
Negative
-
Negative
Negative
Negative
Negative
Negative
Negative
|
-
-
-
-
Neg
Neg
Neg
Neg
|
Recur
SD
Asymp.
Asymp
Asymp
Asymp
Recur
Asymp |
Am Dip PM
Am PM
-
BB Dip
ID
ID
Dig BB ID
Am ID |
|
Proclemer
1993
1
[4] |
65/M |
VF |
no |
RBBB+ST |
Pos |
40 |
VF |
Uncommon trabecular pattern |
Neg |
Recur |
Am ID |
|
Naccarella
1993
1
[5] |
72/M |
NONE |
? |
J wave+ST+LAD |
? |
? |
? |
? |
? |
? |
? |
|
Miyanuma
1993
2
[6] |
47M
39/M |
SPVT/VF,PVC
VF |
? |
IRBBB+ST
J wave + ST |
-
Neg |
? |
-
SPVT/VF |
Negative
Negative |
Neg
Neg
|
SD
Asymp. |
Dysopiramide
Dysopiramide |
|
Sumiyoshi
1993
1
[7] |
42/M |
SPVT/VF |
no |
IRBBB+ST |
- |
normal |
Neg |
Moderately dilated RV and LV |
LV Fib, RV not done |
Asymp |
BB, Mexiletine |
|
Aizawa
1993
1
[8] |
? |
VF |
? |
IRBBB+ST
atypical J wave in V3-V5,
bradycardia dependent |
? |
normal |
? |
Neg |
? |
? |
? |
|
Wiesfeld
1994
1
[9] |
36/M |
VF,PVC |
? |
*IRBBB+ST |
? |
normal? |
AF/AFL |
Normal |
Fib fat |
? |
? |
|
Bjerregaard
1994
1
[10] |
47/F |
SPVT,PVC, Triplets |
no |
J wave+ST |
Neg |
normal |
NSPVT |
Neg |
- |
Asymp |
BB ID |
|
Tada
1994
9
[11] |
All males |
All VF |
? |
"Dynamic right precordial ST elevation" |
? |
) |
? |
5 had RVA |
Neg in all |
? |
? |
|
Ferracci
1994
1
[12 ] |
36 M |
VF |
? |
*IRBB+ST |
Neg |
normal |
neg |
Neg |
Neg |
SPVT/VF |
ID |
|
Nademanee
1995
9
[13] |
? |
all syncope or aborted SD |
? |
* RBBB+ST
(dynamic) |
All Pos |
? |
NSPVT/ VF |
Negative |
? |
2 SD |
? |
|
Naccarella
1996
6
[ 14] |
18/M
53/M
65/M
45/F
29/F
35/M |
VT/VF
VT/VF
NSVT
NSVT
SVT,PVC
SVT,PVC |
YES
YES
YES
YES
YES
YES |
*IRBB+ST+LAD
*IRBB+ST+LAD
*IRBB+ST
*RBBB+ST+LAD
*IRBB+ST+LAD
*IRBB+ST+LAD |
?
?
?
?
?
? |
?
?
?
?
?
^ |
?
?
?
?
?
? |
RVA
RVA
RVA
RVA
RVA
RVA |
-
-
Fib, Fat
Fib, Fat
Fib,Fat
Fb,Fat |
?
?
?
?
?
? |
?
?
?
?
?
? |
|
Corrado
1996
7
[15]
|
?
?
?
?
?
?
? |
None
None (palpit.)
None
None(palpit)
None
None
None |
yes
yes
yes
yes
yes
yes
yes |
J wave+ST
IRBBB+ST+LAD
IRBBB+ST+LAD
IRBBB +ST
IRBBB+ST
loc ST
J wave+ST |
Pos
Pos
Neg
Pos
Neg
Neg
Pos |
-
80
-
-
-
-
- |
-
SMVT (LBBB)
-
-
-
-
- |
RVA
RVA
-
RVA
-
-
RVA |
-
Fib Fat
-
-
-
-
- |
-
Palp
-
Palp
-
-
- |
-
Amio
-
BB
-
-
- |
|
Miyazaki
1996
4
[16] |
29/M
47/M
41/M
38/M |
SMVT (LBBB)
PVC
- (palpit)
VF |
?
?
?
? |
IRBBB+ST+LAD
J wave+ST
J wave+ST
J wave+ST |
Pos
Neg
-
Neg |
100
normal
normal
normal |
SMVT,VF
VF
VF
- |
Negative
Negative
Negative
Negative |
Neg
Neg
-
Neg |
Asymp
Asymp
Asymp
Recur |
BB
Doxasozine
ID
ID Mexiletine |
|
Brugada J
1996
47 (including 8 of ref. 3)
[17] |
? |
32 SPVTand or VF.
-15 asymptomatic |
yes |
*RBBB+ST
(transient in 14) |
? |
? |
32/38 SPVT/VF
|
Negative |
Non speciphic in 16 |
6 SD with 2 macroscopically normal autopsy (no details) |
-22 ID + Amio/ BB
17 Amio/ BB/sotalol
|
|
Gussak
1996
4 (including 1 of ref .10)
[18] |
? |
-1 with VT/VF
-3 asymptomatic |
? |
*J wave |
? |
? |
? |
? |
? |
? |
? |
|
Sheinman
1996
4
[19] |
? |
All had SMVT (LBBB ) |
? |
*2 RBBB+ST
*2 ST |
? |
? |
All inducible VT |
ARVC |
? |
? |
? |
|
Corrado
1996
11
[20] |
All less than 35 years |
All sudden death |
? |
*3 RBBB+ST
*8 ST |
? |
? |
? |
? |
All ARVC at autopsy |
All died suddenly |
? |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
§= Age at the time of the documented episode of aborted sudden death. F=female, M=male. * = ECG trace not published. ? =data not reported. - = not performed. Palp = palpitations. Syn = syncope. RBBB = right bundle branch block. IRBBB = incomplete right bundle branch block (intends r' pattern in V1 aVR with s' in V6). J wave=localized pattern of IRBBB+ST in precordial leads without r' in aVR and s' inV6 (atypical J wave). Pos = positive study. Neg = negative study. MRI = magnetic resonance imaging. LAD= left axis deviation. RV = right ventricle. LV = left ventricle. VT = ventricular tachycardia. NSVT= non sustained ventricular tachycardia. NSPVT = nonsustained polymorphic ventricular tachycardia. SPVT = sustained polymorphic ventricular tachycardia. SMVT = sustained monomorphic ventricular tachycardia. VF = ventricular fibrillation. PVC =premature ventricualr contractions, PPVC = polymorphic ventricular contractions. PRR = polimorphic repetitive response. SR = single response. AF/AFL = atrial fibrillation/flutter. LBBB = left bundle branch block QRS morphology of the ventricular arrhythmia. RVA = right ventricular abnormalities. Fib = fibrosis. Fat = fatty replacement. ARVC = arrhythmogenic right ventricular cardiomyopathy. SD = sudde death. Asymp = asymptomatic. Am = amiodaron, BB = beta-blockers. Dip = diphenylhydantoin. Dig = digitalis. PM = VVI permanent pace-maker. ID = implantable defibrillator
COMPLETE REFERENCE ON THE
SYNDROME OF RIGHT BUNDLE BRANCH BLOCK, ST SEGMENT ELEVATION
AND SUDDEN DEATH
.
- Shipley RA, Hallaran WR. The four lead electrocardiogram in 200 normal men and women. Am Heart J 1936;325-345
- Cannon WB. "Voodoo" death. Am Anthropol 1942, 44: 168-181.
- Osborn JJ. Experimental hypothermia: respiratory and blood pH changes in relation to cardiac function. Am J Physiol 1953;175:389-98
- Hiss RG, Lamb LE, Allen MF. Electrocardiographic findings in 67,375 asymptomatic subjects. X. Normal values. Am J Cardiol 1960, 6: 200-231.
- Hiss RG, Lamb LE, Allen MF. Electrocardiographic findings in 67,375 asymptomatic subjects. X. Normal values. Am J Cardiol 1960, 6: 200-231.
- Wasserburger RH, Alt WJ, Lloyd CJ. The normal RS-T segment elevation variant. Am J Cardiol 1961, 8: 184-192.
- Hersh C. Electrocardiographic changes in head injuries. Circulation 1961;23:853-60
- Hugenholtz PG. Electrocardiographic changes typical for central nervous system disease after right radical neck dissection. Am Heart J 1967;74:438-41
- Parisi A, Beckman C, Lancaster M. The spectrum of ST segment elevation in the electrocardiogram of healthy adult men. J Electrocardiology 1971;4:137-44
- De Sweit J. Changes simulating hypothermia in the electrocardiogram of subarachnoid haemorrhage. J Electrocardiol 1972;5:193-5
- Guerot Cl, Coste A, Valere PE, Tricot R. L' epreuve a l'ajmaline dans le diagnostic du bloc auriculo-ventriculaire paroxystique. Arch Mal Coeur 1973;10:1241-1253.
- Kambara H, Phillips J. Long-term evaluation early repolarization syndrome (normal variant RS-T segment elevation). Am J Cardiol 1976;38:157-61
- Spach MS, Barr RC, Lanning CF, Tucek PC. Origin of body surface QRS and T wave potentials from epicardial potential distributions in the intact chimpanzee. Circulation 1977, 55:268-278.
- Pedersen DH, Zipes DP, Foster RP, Troup PJ. Ventricular tachycardia and ventricular fibrillation in a young population. Circulation 1979;60:988-997
- Morace G, Padeletti L, Porciani M, Fantini F. Effect of isoproterenol on the "early repolarization " syndrome. Am Heart J 1979;97:343-7
- Alimurung BN, Gilbert CA, Felner JM, Schlant RC. The influence of early repolarization variant on the exercise electrocardiogram: A correlation with coronary arteriograms. Am Heart J 1980, 99: 739-745.
- Olsson SB, Edvardsson H, Enestrom S. A case of arrhythmogenic right ventricular dysplasia with ventricular fibrillation. Clin Cardiol 1982;5:591-2
- Virmani R, Rabinowitz M, Clark MA, Mc Allister HA. Sudden death and partial absence of the right ventricular myocardium: a report of three cases and a review of the literature. Arch Pathol Lab Med 1982;106:163-3
- Chiale PA, Przybylski J, Laino RA, et al. Usefulness of the ajmaline test in patients with latent bundle branch block. Am J Cardiol 1982, 49:21-26.
- Chiale PA, Przybylski J, Laino RA, et al. Electrocardiographic changes evoked by ajmaline in chronic Chagas' disease without manifest myocarditis. Am J Cardiol 1982, 49:14-20.
- Marcus FI, Fontaine GH, Guiraudon G. Right Ventricular Dysplasia: A report of 26 Adult cases. Circulation 1982;65:384-397
- Manyari D, Klein G, Gulamhusein S et al. Arrhythmogenic right ventricular dysplasia: a generalized cardiomyopathy? Circulation 1983;68:251-257
- Baron RC, Thacker SB, Gorelkin L. Vernon AA, Taylor WR, Choi K. Sudden death among southeast asian refugees: an unexplained nocturnal phenomenon. JAMA 1983; 250: 2947-2951.
- Benson DW, Benditt DG, Anderson RW et al: Cardiac arrest in young, ostensibly healthy patients: clinical, hemodynamic, and electrophysiologic findings. Am J Cardiol 1983;52:65-69
- Thiene G, Pennelli N, Rossi L. Cardiac conduction system abnormalities as a possible cause of sudden death in young athletes. Human Pathology 1983;14:704-9
- Pietras RJ ,Lam W ,Bauernfeind R et al. Cronic recurrent right ventricular tachycardia in pts without ischemic heart disease:Clinical Hemodynamic and angiographic findings. Am Heart J 1983;105:357-366
- Rowland E , Mc Kenna W , Sugrue D, Barclay R, Foale RA, Krikler DM. Ventricular tachycardia of left bundle branch block configuration in patients with isolated right ventricular dilatation. Clinical and electrophysiological features. Br Heart J 1984;51:15-24
- Fontaine G, Frank R, Guiraudon G. Signification des troubles de conduction intraventriculaires observés dans la dysplasie aventriculaire droite arytmogene. Arch Mal Coeur 1984;77:872-9
- Panidis IP, Greenspan AM, Minz G.S, and Ross J. Inducible ventricular fibrillation in arrhythmogenic right ventricular dysplasia. Am Heart J 1985;110:1067-8
- Saviolo R, Spodick DH. Electrocardiographic responses to maximal exercise during acute pericarditis and early repolarization. Chest, 1986, 90:460-462.
- Rakovec P, Rossi L, Fontaine G et al. Familial arrhythmogenic right ventricular disease. Am J Cardiol 1986; :377
- Maron BJ, Epstein SE, Robert WC. Causes of sudden death in competitive athletes. J Am Coll Cardiol 1986;7:204-14
- Kirschner RH, Echner FAO, Baron RC. The cardiac pathology of sudden unexplained nocturnal death in southeast Asian refugees. JAMA 1986; 256: 2700-2705.
- Gilbert J, Gold RL, Haffajee CI, Alpert JS. Sudden cardiac death in a southeast Asian emigrant; clinical, electrophysiologic, and biopsy characteristics. PACE 1986;9:912-914.
- Deal BJ, Miller SM, Scagliotti D et al. Ventricular tachycardia in a young population without overt heart disease. Circulation 1986;6:1111-1118
- Virmani R, Rabinowitz M. Cardiac pathology and sports medicine. Human Pathology 1987;18:494-501
- Nava A, Scognamiglio R, Thiene G, Canciani B, Daliento L, Boffa GM, Stritoni P. A Polymorphic form of familial arrhythmogenic right ventricular dysplasia. Am J Cardiol 1987;59:1405-1409
- Blomstrom- Lundqvist C, Goran- Sabel KG, Olsson SB. A long term follow up of 15 patients with arrhythmogenic right ventricular dysplasia. Br Heart J 1987;58:477-88
- Belhassen B, Shapira I, Shosani D, Paredes A, Miller H, aniado S: Idiopathic ventricular fibrillation: inducibility and beneficial effect of class I antiarrhythmic agents. Circulation 1987;75:809-816
- Trappe HJ, Brugada P, Talajic M et al. Prognosis of patients with ventricular tachycardia and ventricular fibrillation: role of the underlying etiology. J Am Coll Cardiol 1988;12:166-74
- Thiene G, Nava A, Corrado D, Rossi L, Pennelli N. Right ventricular cardiomyopathy and sudden death in young people. N Engl J Med 1988;318:129-133
- Nava A, Thiene G, Canciani B et al. Familial occurrence of right ventricular dysplasia: a study involving nine families. J Am Coll Cardiol 1988;12:122-8
- Nava A , Scognamiglio R, Buja GF, Daliento L, Bottero Mcanciani B, Corrado D, Stritoni P, Fasoli G, Martini B, Thiene g. Arrhythmogenic right ventricle. Clinical spectrum and familiarity. New trends in Arrhythmias 1986;2:13-19
- Nava A, Canciani B, Scognamiglio R, Buja GF, Daliento L, Miraglia G, Martini B, Thiene G. La tachicardia e la fibrillazione ventricolare nel ventricolo destro aritmogeno. G Ital cardiol 1986;16:741-9
- Nava A, Canciani B, Martini B Buja GF. La ripolarizzazione precoce nelle precordiali destre. Correlazioni ECG-VCG-elettrofisiologia G Ital Cardiol abstract 1988 suppl 1 ;18:118
- Martini B, Nava A, Buja GF, Canciani B, Thiene G. Fibrillazione ventricolarein apparente assenza di cardiopatia. Descrizione di 6 casi. G Ital Cardiol abstract 1988 suppl 1 ;18:136
- Nava A, Canciani B, Schiavinato ML, Martini B, Buja GF. La repolarisation precoce dans le precordiales droites: trouble de la conduction intraventriculaire droite? Correlations de l'electrocardiographie- vectorcardiographie avec l'electro- physiologie. Mises a Jour Cardiologiques 1988;17:157-9
- Nava A, Thiene G, Canciani B, Scognamiglio R, Daliento L, Buja GF, Martini B, Stritoni P, Fasoli G. Familial occurrence of right ventricular dysplasia: a study involving nine families. J Am Coll Cardiol 1988;12:1222-8
- Nava A, Canciani B, Buja GF et al. Electro-vectorcardiographic study of negative T waves on precordial leads in Arrhythmogenic Right Ventricular Dysplasia: relationship with right ventricular volumes. J Electrocardiology 1988;21 (3):239-245
- Nava A, Martini B, Thiene G et al. La displasia aritmogena del ventricolo destro. Studio su una popolazione selezionata. G Ital Cardiol 1988;18:2-9
- Martini B,Nava A, Buja GF et al.Different forms of right ventricular outflow tract tachycardia in 29 patients with right ventricular cardiomyopathy. Eur Heart J 1988;9:17 (abstract)
- Martini B, Nava A, Thiene G, Buja GF, Miraglia G, Scognamiglio R, Boffa GM, Daliento L. Accelerated idioventricular rhythm of infundibular origin in patients with a concealed form of arrhythmogenic right ventricular dysplasia. Br Heart J 1988;59:564-71
- Litovsky SH, Antzelevitch Ch. Transient outward current prominent in epicardium but not endocardium. Circulation Research 1988;62:116-126.
- Belhassem B, Shapira I, Hammerman C. Unusual manifestations of arrhythmogenic right ventricular dysplasia as ventricular fibrillation, atrial paralysis, and hypoexcitable right ventricle. Br Heart J 1988;59:263-5
- Lemery R, Brugada P, Della Bella P, Dugernier T, Wellens H. Ventricular fibrillation in six adults without overt heart disease. J Am Coll Cardiol 1989;13:911-6
- Martini B, Nava A, Thiene G, Buja G.F., Canciani B, Scognamiglio R, Daliento L, Dalla Volta S. Ventricular fibrillation without apparent heart disease: description of six case. Am H J 1989;118;6:1203-9
- Litovsky SH, Antzelevitch Ch. Rate dependence of action potential duration and refractoriness in canine ventricular endocardium differs from that of epicardium: Role of the transient outward current. J Am Coll Cardiol 1989;14:1053-1066.
- Viskin S, Belhassen B. Idiopathic ventricular fibrillation. Am Heart J 1990; 120:661-671
- Krishnan SC, Antzelevitch CH. Sodium channel block produces opposite electrophysiologic effects in canine ventricular epicardium and endocardium. Circulation Research 1991;69:277-291.
- Martini B, Nava A, Thiene G, Buja GF, Canciani B, Miraglia G, Scognamiglio R, Daliento L, Dalla Volta S. Monomorphic repetitive rhythms originating from the right ventricular outflow tract in patients with minor forms of right ventricular cardiomyopathy. Intern J Cardiol 1990;27:211-21
- Litovsky SH, Antzelevitch CH. Differences in the electrophysiologic response of canine ventricular subendocardium and subepicardium to acetylcholine and isoproterenol. A direct effect of acetylcholine in ventricular myocardium. Circulation Research 1990;67:615-627.
- Jain U, Wallis DE, Shah K, Blackeman BM, Moran JF. Electrocardiographic J waves after resuscitation from cardiac arrest. Chest 1990;98:1294-6
- Aihara N, Ohe T, Kamakura S., Matsuhisa M., Takagi H., Shimomura K. Clinical and electrophysiologic characteristics of idiopathic ventricular fibrillation. Shinzo 1990;22 (suppl 2).80
- Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation with normal QT interval and sudden cardiac death. PACE (abstr) 1991;14:746
- Diez U, Schwartze H. Quantitative electrocardiography and vectorcardiography in postnatally developing rats. Journal of Electrocardiology 1991;24:53-62
- Task force of the working group on arrhythmias of the european society of cardiology. The Sicilian gambit; a new approach to the classification of antiarrhythmic drugs based on their actions on arrhythmogenic mechanisms. Circulation 1991;84:1831-51
- Sicouri S, Antzelevitch. A subpopulation of cells with unique electrophysiological properties in the deep subepicardium of the canine ventricle: The M cells. Circ Res 1991, 68:1729-1741
- Suzuki J, Tsubone H, Sugano S. Characteristics of ventricular activation and recovery patterns in the rat. J Vet Med Sci 1992;54:711-716.
- Nava A, Canciani B, Buja GF, Martini B, Scognamiglio R, Daliento L, Oselladore L, Thiene G.. El electrocardiograma y el vectorcardiograma en la dysplasia arritmogénica del ventriculo derecho. Revista Latina de Cardiologia 1992;15:276-83
- Krishnan SC, Antzelevitch C. Flecainide-induced arrhythmia in canine ventricular epicardium. Phase 2 re-entry? Circulation 1992, 87: 562-572.
- Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: A distinct clinical and electrocardiographic syndrome. J Am Coll Cardiol 1992, 20:1391-6.
- Martini B, Nava A, Canciani B, Thiene G. Right bundle branch block, persistent ST segment elevation and sudden cardiac death . (letter) J Am Coll Cardiol 1993;22:633
- Aizawa Y, Tamura M, Chinushi M, et al. An attempt at electrical catheter ablation of the arrhythmogenic area in idiopathic ventricular fibrillation. Am Heart J 1992, 123: 257-260.
- Sumiyoshi M, Nakata Y, Hisaoka T, Ogura S, Nakazato Y, Kawai S, Okada R, Yamaguchi H. A case of idiopathic ventricular fibrillation with incomplete right bundle branch block and persistent ST segment elevation. Jpn Heart J 1993;34:661-666
- Proclemer A, Facchin D, Feruglio GA, Nucifora R. Fibrillazione ventricolare recidivante, blocco di branca destra, persistent sopraslivellamento del tratto ST in V1-V3: una nuova syndrome aritmica? Descrizione di un caso clinico. G Ital Cardiol 1993,23: 1211-1218.
- Naccarella F. Malignant ventricular arrhythmias in patients with a right bundle branch block and persistent St segment elevation in V1-V3: A probable arrhythmogenic cardiomyopathy of the right ventricle. G Ital Cardiol 1993, 23: 1219-1222.
- Brugada P, Brugada J. Do not get confused, please. G Ital Cardiol 1993
- Miyanuma H, Sakurai M, Odaka H, Yamazaki T., Mitobe H., Muraguti I, Iwama N. Two cases of idiopathic ventricular fibrillation with interesting electrocardiographic findings. Kokyu to Junkan 1993;41:287-91
- Brugada P, Geelen P, Brugada J. Further observations on the syndrome of right bundle branch block, persistent ST segment elevation and sudden cardiac death. N Trends Arrhythmias 1994;9:333-4
- Aizawa Y, Tamura M, Chinushi M, Naitoh N, Uchiyama H, Kusano Y, Hosono H, Shibata A. Idiopathic ventricular fibrillation and bradycardia-dependent intraventricular block. Am Heart J 1993;126:1473-4
- Wu MH, Su MJ, Leu HC. Age-related quinidine effects on ionic currents in rabbit cardiac myocytes. J Mol Cell Cardiol 1994;26:1167-1177.
- Wiesfeld AC, Crijns GM, Van Dijk RB et al. Potential role of endomyocardial biopsy in the clinical characterization of patients with idiopathic ventricular fibrillation: Arrhythmogenic right ventricular dysplasia- an undervalued cause. Am Heart J 1994;127;1421-4
- Tada H, Aihara N, Ohe T, Yutani C, Shimizu W, Kurita T, Kamakura s, Shimomura K. New insight in idiopathic ventricular fibrillation patients with right precordial ST segment elevation. Circulation 1994;90:1511 (abstract)
- Leenhardt L, Glaser E, Burguera M, et al. Short-coupled variant of torsade de pointes: A new electrocardiographic entity in the spectrum of idiopathic ventricular arrhythmias. Circulation 1994;89:206-215.
- Spach M. Changes in the topology of gap junctions as an adaptive structural response of the myocardium. Circulation 1994; 90: 1103-1105.
- Sao N, Akasaka K, Kawashima E, et al. A case of idiopathic ventricular fibrillation with possible mechanism of autonomic dysfunction. Jpn J Electrocardiol 1994, 14: 206-217.
- Peters N, Severs N, Rothery S, Lincoln C, Yacoub M, Green C. Spatiotemporal relation between gap junctions and fascia adherens junctions during postnatal development of human ventricular myocardium. Circulation 1994;90:713-725.
- Moise NS, Meyers-Wallen V, Flahive WJ, et al. Inherited ventricular arrhythmias and sudden death in german shepherd dogs. J Am Coll Cardiol 1994, 24: 233-243.
- Leenhardt A, Thomas O, Bel A, Bizot J, Coumel P, Slama R. Le defibrillateur automatique implantable: Resultats a long terme. Arch Mal Coeur 1994, 87: 1617-1622.
- James TN. Normal and abnormal consequences of apoptosis in the human heart. Circulation 1994;90:556-573.
- Hojo Y, Yamasawa M, Ichida M et al. Polymorphic recurrent ventricular tachycardia with bizarre QRS wave prevented by sympathomimetic agents. Shinzoh 1994, 26: 540-545.
- Ferracci A, Fromer M, Schlapfer J, Pruvot E, Kappemberger L. Fibrillation ventriculaire primitive et recidive precoce; à propos d'un cas associant bloc de branche droit et sus-décalage persistant du segment ST. Arch Mal Coeur 1994;87:1359-1362
- Dixon JE, Mckinnon D. Quantitative analysis of potassium channel mRNA expression in atrial and ventricular muscle of rats. Circulation Research 1994;75:252-260.
- Coumel P, Le Marec H. Puppies' programmed sudden death: Who is the serial killer? J Am Coll;Cardiol 1994, 24: 244-246.
- Bjerregaard P, Gussak I, Kotar S, Gessler JE, Janosik D. Recurrent syncope in a patient with prominent J wave. Am Heart J 1994;127:1426-30
- Nakazawa K, Matsumoto N, Takenobu H, Akagi T, Miyake H, Murayama M. Characteristic of idiopathic ventricular fibrillation with reference to electrocardiographic morphology of RBBB and St elevation. Heart (Jpn) 1994;26:2631
- Nakazawa K, Matsumoto N, Akagi T et al. Analysis of the role of the autonomic nervous system in near sudden death cases due to idiopathic ventricular fibrillation. Ther Res 1994;15:52-6
- Viskin S , Belhasssen B. When you only live twice. N Engl J Med 1995;332:1221-1225.
- Namiki T, Ogura T, Kuwabara Y, Kobayashi S, Saito T, Masuda Y. Five-year mortality and clinical characteristics of adult subjects with right bundle branch block with ST elevation. Circulation 1995;92:1591 (abstract)
- Nademanee K, Veerakul G, Nimmanit S, Tungsanga K, Chaowakul V, Malasit P. Right bundle branch block and ST segmente elevation, an arrhythmohgenic marker for sudden unexpected death syndrome in young Thai men. Circulation 1995;92:1596 (abstract)
- Martini B, Basso C, Thiene G. Sudden death in mitral valve prolapse with Holter monitoring-documented ventricular fibrillation: evidence of coexisting arrhythmogenic right ventricular cardiomyopathy. International Journal of Cardiology 1995;49:274-8
- Marcus FI, Fontaine G. Arrhythmogenic right ventricular dysplasia/cardiomyopathy. PACE 1995;18:1298-1313
- Li GR, Feng J, Wang Z, et al. Comparative mechanisms of 4-aminopyridine-resistant Ito in human and rabbit atrial myocytes. Am J Physiol 1995;269:463-472.
- Le Grand B, Marty A, Colpaert FC. Katenserin inhibits the transient outward current in rabbit ventricular myocytes. J Cardiovasc Pharmacol 1995;25:341-344.
- Gussak I, Bjerregaard P, Egan T, Chaitman B. ECG phenomenon called the J wave. Journal of Electrocardiology. 1995;28:49-58
- Nakazawa K, Murayama M. The significance of autonomic nervous tone with idiopathic ventricular fibrillation in patients with RBBB with St segment elevation on the ECG. Heart (Jpn) 1995;27:364-73
- Drouin E, Charpentier F, Gauthier Ch, Laurent K, Le Marec H. Electrophysiologic characteristics of cells spanning the left human heart: Evidence for presence of M cells. J Am Coll Cardiol 1995;26:185-192.
- D'Onofrio A, Cuomo S, Musto B, Boccalatte A. Right bundle branch block, persistent ST segment elevation in V1-V3 and sudden cardiac death: always a distinct syndrome? G Ital Cardiol 1995;25:1171-1175.
- Corrado D. Thiene G, Nava A, Rossi L., Pennelli N. Sudden death in young competitive athletes: clinico-pathologic correlations in 22 cases. Am J Med 1995;89:588-96
- Clark RB, Sanchez-Chapula J, Slinas-Stefanon E, et al. Quinidine-induced open channel block of K+ current in the rat ventricle. Br J Pharmacol 1995;115:335-343.
- Chambers JW, Denes P, Dahl, W, et al. Familial sudden death syndrome with an abnormal signal-averaged electrocardiogram as a potential marker. Am Heart J 1995;130:318-323.
- Brugada J, Brugada P. Right bundle branch block, ST segment elevation and sudden cardiac death: Symptomatic, asymptomatic, and intermittent forms. PACE (abstract) 1995, 18: 951.
- Tohyou Y, Nakazawa K, Ozawa A et al. A survey in the incidence of right bundle branch block with ST segment elevation in among normal population. Jpn J Electrocardiology 1995;15:223-6
- Yamashita T, Nakajima T, Hamada H, et al. Flecainide inhibits the transient outward current in atrial myocytes isolated from rabbit heart. J Pharmacol Exp Ther 1995;274:315-321.
- Evans GT. Electrocardiographic predictors of cardiac rhythm disturbances. In Braunwald E (ed). Atlas of Heart Diseases. Vol IX. Arrhythmias: Electrophysiologic principles. Current Medicine 1996, p 3.9
- Zespof Brugadow. (in polish) Electrofisjol I Stymul Serca 1996;3: 315-320.
- Yan GX, Antzelevitch C. Cellular basis for the electrocardiographic J wave. Circulation 1996;93:372-9
- Veerakul G, Nademanee K. Dynamic changes in the RBBB and ST elevation in the right precordial leads observed in patiets with idiopathic rventricular fibrillation: evidence of phase 2 repolarization abnormality (abstr) Circulation 1996;92 Suppl:i-626;#3669
- Villacorta H, Faig Torres RA, Ribeiro Simoes de Castro I, Lambert H, de Araujo Gonzales Alonso R. Sudden death in patient with right bundle branch block and persistent ST segment elevation. Arq Bras Cardiol 1996;66:229-231.
- Sumita S, Miyazaki T, Ishikawa T et al. ST level in healthysubject with Right bundle branch block in relation to Brugada syndrome (abstract. Eur J Pacing Electrophysiology 1996;6:270:#1076
- Shimada M, Miyazaki T, Miyoshi S, et al. Sustained monomorphic ventricular tachycardia in a patient with Brugada syndrome. Jpn Circ J 1996;60:364-370.
- Sheinman MM. Right bundle branch block and ST Elevation is not a distinct syndrome identifying patients at risk for sudden cardiac death. European Journal of Cardiac Pacing and Electrophysiology 1996;6:7 (abstract)
- Brugada P, Brugada J. Right bundle branch block, ST segment elevation and sudden cardiac death. Symptomatic and asymptomatic and intermittent forms. JACC 1995;25:95A (abstract)
- Brugada P, Brugada J. Right bundle branch block, ST segment elevation and sudden cardiac death. Symptomatic and asymptomatic and intermittent forms. Eur J C P E 1996;6:130 (abstract)
- Naccarella F, Mezzetti M, Palmieri M, Barbato G, Medda M, Di Niro MR, Cavallari F, Masotti A, Bracchetti D, Nanni G, Rimondini R. Analysis of the ECG pattern "incomplete right bundle branch block and ST elevation in V1 V3 in different clinical subsets. A primary electrical disease or an early high right anteroseptal involvement as in right ventricular dysplasia-cardiomyopathy? Preliminary results. New Trends Arrhythmias 1996;9:405-8
- Nademanee K, Sudden unexpected death syndrome in young Thai men. Eur JCPE (abstract) 1996, 6: 130.
- Miyazaki T, Mitamura H, Miyoshi S, Soejima K, Aizawa Y, Ogawa S. Autonomic and antiarrhythmic modulation of ST segment elevation in patients with Brugada syndrome. J Am Coll Cardiol 1996, 27: 1061-1070.
- Kobayashi T, Shintani U, Yamamoto T, et al. Familial occurrence of electrocardiographic abnormalities of the Brugada-type. Intern Med 1996;35:637-640.
- Gussak I, Bijerregaard P, Chaitman B. ECG phenomenon called J wave: from hypothermia to Brugada syndrome. European Journal of Cardiac Pacing and Electrophysiology 1996;6:130 (abstract)
- Fontaine G. Familial cardiomyopathy associated with right bundle branch block, ST segment elevation and sudden death. J Am Coll Cardiol 1996;28:540-541 (letter).
- Fontaine G, Piot O, Sohal P et al. Derivations en precordiales droites et mort subite. Arch Mal Coeur 1996, 89: 1323-1329.
- Villacorta H, Faig Torres RA, Ribeiro Simoes de castro I, Lambrert H, de Araujio GAR. Sudden death in a patient with right bundle branch block and persistent ST segment elevation. Arq Bras Cardiol 1996;66:229-31
- Corrado D, Basso C, Buja GF, Nava A, Thiene G . Right bundle branch block, persistent right precordial St segment elevation, and sudden arrhythmic death in young people. PACE (abstract) 1996, 19:669.
- Corrado D, Basso C, Nava A, Buja GF, Thiene Gl. Right bundle branch block, persistent right precordial St segment elevation, and sudden arrhythmic death in young people. Eur Heart J 1996;17:211 (abstract)
- Corrado D, Basso C, Buja GF, Nava A, Thiene G Pathologic substrates of right bundle branch block, persistent right precordial ST segment elevation, and sudden death in young people. EUR J C P E 1996;6:36 (abstract).
- Corrado D, Nava A, Buja GF, Martini B, Fasoli G, Oselladore L, Turrini P, Thiene G. Familial cardiomyopathy underlies syndrome of right bundle branch block, ST segment elevation and sudden death. J Am Coll Cardiol 1996;27:443-8
- Ohe T. Idiopathic ventricular fibrillation of the Brugada type: an atypical form of arrhythmogenic right ventricular cardiomyopathy? Intern Med 1996;35:595 (editorial).
- Brugada J, Brugada P. What to do in patients with no structural heart disease and sudden arrhythmic death? Am J Cardiol 1996;78(suppl 5a):69-75
- Fontaine G, Piot O, Sohal P. Right precordial leads and sudden death. Relations with arrhythmogenic right ventricular dysplasia. Arch Mal Coeur Vaiss 1996;89:1323-9
- Brugada J, Brugada P, Brugada R. Ajmaline unmasks right bundle branch block-like and ST segment elevation in V1-V3 in patients with idiopathic ventricular fibrillation. PACE (abstract) 1996,19: 599.
- Aizawa Y, Naitoh N, Washizuka T, Takahashi K, Uchiyama H, Shiba M, Shibata A. Electrophysiological findings in idiopathic recurrent ventricular fibrillation. PACE 1996, 19: 929-939.
- Douard H et al. Fortuitous discovery of Brugada Syndrome in an asymptomatic 70-year-old sportman. Ann Cardiol Angeiol 1996;45:577-80
- Naccarella F, Accorsi A, Palmieri M, Barbato G, Bracchetti D, Nanni G, Rimondini R. Aspetti elettrocardiografici a tipo BBDx incompleto ed ST sopraslivellato in V1-V3. Un marker specifico di sindromi aritmiche severe o di displasia destra iniziale?. Atti SIC Sport
- Atarashi H, Ogawa S, Harumi K, et al. Characteristics of patients with right bundle branch block and ST segment elevation in right precordial leads. Am J Cardiol 1996;78:581-3
- Tohyo Y, Nakazawa K, Matsumoto N, Masui Y, Sakurai T, Murayama M. Significance of QT dispersion in right bundle branch block, ST elevation and sudden death syndrome. PACE (abstract) 1997;20: 1469.
- Martini B, Corrado D, Nava A, Thiene G. Syndrome of Right bundle branch block, st segment elevation and sudden death. Evidence of an organic substrate. In Nava A, Rossi L and Thiene G editors: Arrhythmogenic right ventricular cardiomyopathy/dysplasia. Elsevier 1997:438-53
- Brugada J, Brugada P, Brugada R. Apparent Right bundle branch block, st segment elevation and sudden cardiac death. In Nava A, Rossi L and Thiene G editors: Arrhythmogenic right ventricular cardiomyopathy/dysplasia. Elsevier 1997:428-37
- Spodick DH. Early repolarization: An underinvestigated misnomer. Clin Cardiol 1997 ,20:913-914.
- Scheinman MM. Is the Brugada syndrome a distinct clinical entity? J Cardiovasc Electrophysiol 1997, 8: 332-336.
- Lorga Filho A, Primo J, Brugada P, Brugada J. Right bundle branch block, st segment elevation of the st segment in V1 to V3 and sudden cardiac death.: the diagnostic and therapeutic approach. Rev Port Cardiol 1997;16:443-7
- Nakazato Y, Shimada K, Nakazato K, et al. Abnormal ST elevation during oral pilsicainide treatment. Ther Res (in japanese) 1997;18:357-362.
- Nakazato Y, Nakata Y, Yasuda M, et al. Safety and efficacy of oral flecainide acetate in patients with cardiac arrhythmias. Jpn Heart J 1997;38:379-385.
- Nademanee K,K, Veerakul G, Nimmannit S. Arrhythmogenic marker for the sudden unexplained death syndrome in Thai men.Circulation 1997, 96:2595-2600.
- Nademanee K, Sudden unexpected death syndrome in Southeast Asia. Am J Cardiol 1997;79:10-1
- Naccarella F, Barbato G, Palmieri M, Lepera G, Bracchetti D. Familial distribution of the incomplete bundle branch block, ST segment elevation and sudden death syndrome. A clinical-morphologic and genetic study of five families. PACE 1997, 20: 1213.
- Myerburg RJ, Basset AL. Cellular electrophysiology, heterogeneity, and arrhythmias. J Cardiovasc Electrophysiol 1997;8:884-886.
- Di Diego, Antzelevich C. Ica inhibition and IK-ATP activation induce a transmural dispersion of repolarization resulting in ST segment elevation and arrhythmias. Abstract PACE 1998;19 (suppl).577
- Brugada P, Brugada J, Brugada R. Brugada Syndrome: A structural cardiomyopathy or a functional electrical disease? In Raviele A editor: Cardiac Arrhythmias 1977 Springer- Verlag Milano 1998 pag. 323-332
- Morgera T, Sinagra GF, Viel E, Ricci C, Bussani R, Camerini F. The syndrome of right bundle branch block, persistent ST segment elevation and sudden cardiac death. Which is the histological substrate? Eur Heart J (letter to the Editor) 1997, 18: 1190-1191.
- Marcus FI. Idiopathic ventricular fibrillation. J Cardiovasc Electrophysiol 1997, 8: 1075-1083.
- Kasanuki H, Ohnishi S, Ohtuka M, et al. Idiopathic ventricular fibrillation induced with vagal activity in patients without obvious heart disease. Circulation 1997, 95: 2277-2285.
- Inagaki M, Sugimachi M, Tatewaki. Dynamic response of right precordial ST- elevation to changes in cycle length in patients with idiopathic ventricular fibrillation. Circulation (abstract) 1997.
- Hata Y, Chiba N, Hotta K, et al. Incidence and clinical significance of right bundle branch block and ST segment elevation in V1-V3 in 6- to 18-year-old school children in Japan. PACE (abstract) 1997, 20: 2310.
- Freeman LC, Pacioretty LM, Moise NS, Kass RS, Gilmour RF.Decreased density of Ito in left ventricular myocites from german shepherd dogs with inherited arrhythmias. J Cardiovasc Electrophysiol 1997, 8: 872-883.
- Chinushi M, Aizawa Y, Ogawa Y, Shiba M, Takahashi K. Discrepant drug action of disopyramide on ECG abnormalities and induction of ventricular arrhythmias in a patient with Brugada syndrome. Journal of Electrocardiography 1997, 30: 133-134.
- Brugada P, Brugada J, Brugada R. "Brugada syndrome" : A structural cardiomyopathy or a functional electrical disease? In: Raviele , ed. Cardiac Arrhythmias. Springer-Verlag 1997.
- Brugada J, Brugada R, Brugada P. Right bundle branch block, ST segment elevation in leads V1-V3: A marker for sudden death in patients without demonstrable structural heart disease. Circulation (abstract) 1997, 96: 151.
- Brugada J, Brugada J. Further characterization of the syndrome of right bundle branch block, ST segment elevation and sudden cardiac death. J Cardiovasc Electrophysiol 1997, 8: 325-331.
- Brembilla-Perrot B, Beurrier D, Jacquemin L, et al. Incomplete bundle branch block and ST-segment elevation: syndrome associated with sustained monomorphic ventricular tachycardia in patients with apparently normal heart. Clin Cardiol 1997;20:407-410.
- Bolognesi R, Tsialtas D, Vasini P, Conti M, Manca C. Abnormal ventricular repolarization mimicking myocardial infarction after heterocyclic antidepressant overdose. Am J Cardiol 1997,79: 242-245.
- Antzelevitch Ch, Sicouri S, Litovsky SH, et al. Heterogeneity within the ventricular wall. Electrophysiology and pharmacology of epicardial, endocardial and M cells. Circulation Research 1997.
- Aihara N, Takaki H, Taguchi A. Exercise induced aggravation of ST segment elevation in patients with Brugada type idiopathic ventricular fibrillation. Circulation 1997. Abstract.
- Hirata K, et al Beat-to -bet variation of the ST segment in a patient with right bundle branch block, persistent ST segment elevation, and ventricular fibrillation: a case report. Angiology, 1998;49:87-90
- Zarco P. Sindrome del QT largo. Eur Cardiol Fax 1998; 21-9-98.
- Corrado D, Basso C, Buja GF, Nava A. Right Bundle Branch Block, right precordial ST segment elevation and sudden death in the young. Round table: About so called Brugada and Martini-Nava syndromes G Ital Cardiol 1998;28 suppl 1:566-8
- Corrado D, Basso C, Buja GF, Nava A, Thiene G. Right Bundle Branch Block, right precordial ST segment elevation and sudden death. Elecrocardiographic and pathologic correlations. Circulation 1998;31:293A abstract
- Corrado D, Turrini P, Basso C, Buja GF, Nava A, Thiene G.QT dispersion right precordial ST ST segment elevation and sudden death in arrhythmogenic right ventricular cardiomyopathy. JACC 1998;31:131A abstract
- Brugada J, Brugada R, Brugada P. Right bundle branch block, ST segment elevation in leads V1-V3and sudden cardiac death. Round table: About so called Brugada and Martini-Nava syndromes. G Ital Cardiol 1998;28 suppl 1:568-71
- Naccarella F, Rolli A, Carboni A et al. Further observations of the Brugada-Martini syndrome. Familial distribution of the incomplete bundle branch block, STT elevation and sudden death syndrome. A clinical-morphologic and genetic study of nine families. Round table: About so called Brugada and Martini-Nava syndromes. G Ital Cardiol 1998;28 suppl 1:571-4
- Yan GX, Shimizu W, Antzelevitch C. Characteristics and distribution of M cells in arterially perfused canine left ventricular wedge preparations. Circulation 1998;98:1921-1927.
- Weiss R, London B, McNamara D, et al. Familial occurrence of right bundle branch block, ST elevation, and arrhythmia susceptibility. PACE 1998; 21:939.
- Rook M, Aishinawi C, Groenewegen A, et al. Human SCN5A gene mutations alter Na-current kinetics and associate with VF in patients without structural heart disease. Circulation 1998; abstract 2461.
- Washizuka T, Chinushi M, Niwano S, Aizawa Y. Bifid T waves induced by isoprenaline in a patient with Brugada syndrome. Heart 1998; 79:305-307.
- Littman L. Bifid T waves induced by isoprenaline in a patient with Brugada syndrome. Heart 1998;80:633. (Letter).
- Washisuka T, Chinushi M, Niwano S, et al. Reply letter to previous. Heart 1998;80:633
- Viskin S, Belhassen B. Increased vagal activity in idiopathic VF. Circulation 1998;97:937-8
- Vergara I, Wharton JM. Ventricular tachycardia and fibrillation in normal hearts. Current Opinion in Cardiology 1998;13:9-19.
- Thomas SA, Schuessler RB, Berul CI, et al. Disparate effects of deficient expression of connexin 43 on atrial and ventricular conduction. Circulation 1998;97:686-691.
- Tagaki M, Aihara N, Taguchi A, et al. Localized right ventricular morphological abnormalities in patients with Brugada syndrome by ultrafast computed tomography and magnetic resonance imaging. Is Brugada syndrome truly idiopathic? Circulation 1998, abstract 848.
- Tada HT, Aihara N, Ohe T, et al. Arrhythmogenic right ventricular cardiomyopathy underlies syndrome of right bundle branch block, ST- segment elevation, and sudden death. Am J Cardiol 1998;81:519-522.
- Rudski MB. Right bundle branch block, persistent ST- segment elevation, and sudden death. Letter of reply. Am J Cardiol 1998;82:407-8
- Bertaglia E, Michieletto M, Spedicato L, Pacotto P. Brugada P, Brugada J. Right bundle branch block, intermittent ST- segment elevation, and inducible ventricular tachycardia in an asymptomatic patient: an unusiual presentation of Brugada Syndrome. G Ital cardiol 1998;28:893-8
- Brugada R, Roberts R. The molecular genetics of arrhythmias and sudden death. Clin Cardiol 1998;21:547-54
- Viskin S, Belhassem B. Polymorfic ventricular tachyarrhythmias ihn the absence of organic heart disease: classification, differential diagnosis, and implications for therapy. Progress Cardiv Dis 1998;41:17-34
- Stephan E, Chedid R, Loisele J, Bouvagnet P. Genetique clinique et moleculaire d'un bloc de branche familial lie au chromosome 19. Arc Mal Coeur 1998; 91:1465-1474.
- Teo WS, et al. The Brugada syndrome in a chinese population. In J Cardiol 1998;65:281-6
- Nakamura M, et al. Incessant ventricular fibrillation attacks in a patient with Brugada syndrome. Int J Cariol 1998;64:205-6
- Corrado D, Basso C, Buja GF, Nava A, Thiene G. Electrocardiographic and pathologic correlations in the syndrome of right bundle branch block, right precordial ST segment elevation and sudden death. Eur H J 1998;18 (suppl) 577 abstract
- Peters NS, Wit AL. Myocardial architecture and ventricular arrhythmias. Circulation 1998; 97:1746-1754.
- Nomura M, Nada T, Endo J, et al. Brugada syndrome associated with an autonomic disorder. Heart 1998;80:194-196.
- Cheng T O. Brugada syndrome associated with autonomic disorde. Heart 1999;81:330 (letter of answer)
- Nakamura W, Segawa K, Ito H, Tanaka S, Yoshimoto N. Class Ic antiarrhythmic drugs, flecainide and pilsicainide, produce ST segment elevation simulating inferior myocardial ischemia. J Cardiovasc Electrophysiol 1998; 9:855-858.
- Arsenjo R, et al. Sudden death due to recuperated ventricular fibrillation: Brugada syndrome?. Rev Med Chil 1998;126:814-21
- Nava A, Martini B, Bauce B, Corrado D, Naccarella F. La sindrome blocco di branca destra, sopraslivellamento precordiale del tratto ST e morte improvvisa è una alterazione strutturale o funzionale?. Quale terapia?. In Alboni P editor: Controversies in arrhythmology. TipoLito Italia SNC 1998
- Nakagawa T, Aihara N, Taguchi A, et al. ST segment alternans in patients with Brugada type idiopathic ventricular fibrillation during ambulatory ECG recordings. PACE 1998; 21: 967.
- Takagi M, Aihara N, Taguchi A, Matsua K, Suyama K, Kurita T, Kamakura S, Hamada S. Localized right ventricular morphological abnormalities in patients with Brugada syndrome by ultrafast computed tomography and magnetic resonance imaging. Is Brugada syndrome truly idiopathic. Circulation 1998 (suppl I-1) 164
- Corrado D, Turrini P, Buja GF, Basso C, Nava A, Thiene G. QT dispersion right precordial ST segment elevation and sudden death in arrhythmogenic right ventricular cardiomyopathy. Abstract JACC 1998;31 (suppl A)131-A
- Corrado D, Basso C, Buja GF, Nava A, Thiene G. Right bundle branch block , right precordial ST segment elevation and sudden death.Electrocardiographic and pathologic correlations. Abstract JACC 1998;31 (suppl A):293A
- Corrado D, Basso C, Buja GF, Nava A, Thiene G. Electrocardiographic and pathologic correlation in the syndrome of right bundle branch block, ST segment elevation and sudden death. Abstract Eur H J 1998;19 (suppl):577
- Brugada J, Brugada R, Wang Q, Potenza D, Towbin J, Brugada P. Unmasking of genotypic and fenotypic abnormalities by the administration of class I antiarrhythmic drugs in patients with sudden death and structurally normal hearts. Eur H J 1998;19 (suppl):577
- Muller-Ehmsen J , Brixius K, Schwinger RH. Positive inotropic effects of the novel Na+- channel modulator BDF 9198 in human nonfailing and failing myocardium. J Cardiovasc Pharmacol 1998;31: 684-689.
- McNamara D, Weiss R. Molecular heterogeneity in the Brugada syndrome. Circulation 1998, abstract 2400.
- Matsuo K, Shinizu W, Kurita T Inagaki M, Aihara N, Kamakura S. Dynamic changes of 12-lead electrocardiograms in a patient with Brugada syndrome. J Cardiovasc Electrophysiol 1998;9:508-512.
- Matsuo K, Shimizu W, Kurita T, et al. Increased dispersion of repolarisation time determined by monophasic action potentials in two patients with familial idiopathic ventricular fibrillation. J Cardiovasc Electrophysiol 1998, in press..
- Matsuo K, Inagaki M, Kurita T, et al. Long-term temporal and circadian patterns of ventricular fibrillation after cardioverter-defibrillator implantation in patients with Brugada syndrome. PACE 1998; 21:891.
- Makita N, Shirai N. Mutant Cardiac Na+ channel alpha subunit (T1620M) of an idiopathic ventricular fibrillation family exhibits altered functional association with beta1 subunit. Circulation 1998;abstract 275.
- Krishnan SC, Josephson ME. ST segment elevation induced by class Ic antiarrhythmic agents. J Cardiovasc Electrophysiol 1998;9:1167-1172.
- Kondo K, Watanabe I, Kojima T, et al. Role of programmed electrical stimulation in the syndrome of right bundle branch block, ST segment elevation. PACE 1998;21:820.
- Kasanuki H, Matda N, Ohnishi S. Increased vagal activity in idiopathic VF. Circulation 1998; 97: 938-940.
- Kakishita M, Kurita T, Matsuo K, et al. Mode of spontaneous onset of ventricular fibrillation in patients with idiopathic ventricular fibrillation detected by implantable cardioverter defibrillator therapy. Circulation 1998, abstract 1510.
- Ikeguchi S, Hashimoto T, Horie M, Sasayama S. A case of Wolff-Parkinson-White syndrome associated with asymptomatic Brugada syndrome and sudden death. PACE, 1998, in press.
- Hurst W. Naming of the waves in the ECG, with a brief account of their genesis. Circulation 1998;98:1937-1942.
- Goethals P, Debruyne P, Saffarian M. Drug-induced Brugada syndrome. Acta Cardiol 1998; 53:157-160.
- Garg A, Finneran W, Feld GK. Familial sudden cardiac death associated with a terminal QRS abnormality in surface 12-lead electrocardiogram in the index case. J Cardiovasc Electrophysiol 1998; 9:642-647.
- Fontaine G, Fontaliran F, Frank R. Arrhythmogenic right ventricular cardiomyopathies. Circulation 1998;97:1532-1535.
- Eriksson P, Hansson PO, Eriksson H, Dellborg M. Bundle-branch block in a general male population . The study of men born in 1913. Circulation 1998;98:2494-2500.
- Engelstein ED, Zipes D. Sudden cardiac death. In: Hurst' s The Heart. Alexander RW, Schlant RC, Fuster V (eds.); Mc Graw-Hill 1998. p1081-1112.
- Marcus FI. Letter to the Editor. J Cardiovasc Electrophysiol 1998.
- Corrado D, Basso C, Buja G, Nava A, Thiene G. Right bundle branch block; right precordial ST segment elevation, and sudden death: Electrocardiographic and pathologic correlations. J Am Coll Cardiol 1998; 293A (abstract).
- Coonar AS, Protonotarios N, Tsatsopoulou A, et al. Gene for arrhythmogenic right ventricular cardiomyopathy with diffuse nonepidermolytic palmoplantar keratoderma and woolly hair (Naxos disease) maps to 17q21. Circulation 1998; 97:2049-2058.
- Condo K, Watanabe I, Kojima T, et al. Role of programmed electrical stimulation in the syndrome of right bundle branch block, ST segment elevation. PACE 1998, in press.
- Chen Q, Kirsch GE, Zhang D, Brugada R, et al. Genetic basis and al. Molecular mechanisms for idiopathic ventricular fibrillation. Nature 1998, 392;293-296
- Burke A, Arbustini E, dal Bello B, Morbini P, Specchia G, Virmani R. Fat infiltrates in endomyocardial biopsies lack specificity for the diagnosis or right ventricular dysplasia. J Am Coll Cardiol 1998;68A (abstract)
- Brugada R. Bases geneticas de las arritmias. Rev Esp Cardiol 1998;51:274-285.
- Brugada J, Brugada R, Brugada P. Sindrome del bloqueo de rama derecha, elevacion del segmento ST en V1 a V3 y muerte subita cardiaca. Rev Esp Cardiol 1998, in press.
- Brugada J, Brugada R Brugada P. Right bundle branch block and ST segment elevation in leads V1-V3: A marker for sudden death in patients with no demonstrable structural heart disease. Circulation 1998, 97:457-460.
- Bourke JP, Doig JC. Ventricular tachyarrhythmias in the normal heart. Futura Publishing Co.Armonk, New York 1998, p 51-57.
- Bjerregaard P, Gussak I, Antzelevitch C. The enigmatic manifestation of Brugada syndrome. J Cardiovasc Electrophysiol 1998, in press.
- Barinaga M. Tracking down mutations that can stop the heart. Science 1998;281:32-34.
- Antzelevitch C. The Brugada syndrome. J Cardiovasc Electrophysiol 1998, 9: 513-516.
- Alexander RW, Schlant RC, Fuster V. The Heart. Mc Graw Hill 1998; p 1094.
- Ahmad F, Li D, Karibe A, et al. Localization of a gene responsible for arrhythmogenic right ventricular dysplasia to chromosome 3p23. Circulation 1998;98:2791-2795.
- Alshinawi C, Mannens M, Wilde A. Mutations in the human sodium channel gene (SCN5A) in patients with Brugada syndrome. Eur Heart J 1998;19:78 (Abstract)
- Rook MB, Alshinawi C, Groenewegen WA et al. Human SCN5A gene mutation alter Na-current kinetics and associate with VF in patients without structural heart disease. Circulation 1998;98 (suppl):1-468 (Abstract)
- Forleo C, Pitzalis MV, Rizzon P. Cardiomiopatia aritmogena del ventricolo destro. Cardiologia 1998;43:1287-1304
- Wilde A, Duren D. Sudden cardiac death, RBBB, and rightprecordial ST-segment elevation. Circulation 1999;99:722-3 (letter).
- Brugada J, Brugada R, Brugada J. Reply to letter of Wilde. Circulation 1999;99:723
- Priori SG, Napolitano C, Schwartz PJ. Low penetrance in the long QT syndrome. Clinical impact. Circulation 1999;99:529-533.
- Priori SG, et al. Genetic and molecular basis of cardiac arrhythmias. Impact on clinical management. Parts I and II. Circulation 1999;99:518-528.
- Priori SG, Barhanin J, Hauer RNW, et al. Genetic and molecular basis of cardiac arrhythmias. Eur Heart J 1999;20:174-195.
- Priori SG et al. Genetic and molecular basis of cardiac arrhythmias. Impact on clinical management. Part III
- Alings M, Wilde A. "Brugada" syndrome. Clinical data and suggested pathophysiological mechanism. Circulation 1999;99:666-673.
- Gussak I, Antzelevitch C, Bjerregaard P, Towbin J, Chaitman BR. The Brugada syndrome: Clinical, Electrophysiologic and Genetic Aspects. J Am Coll Cardiol 1999;33:5-15
- Brugada P, Brugada J, Brugada R. Sudden death in relatives and patients with the syndrome of right bundle branch block and ST segment elevation from V1 to V3. J Am Coll Cardiol 1999, abstract
- Matsuo K, Kurita M, Inagaki M, et al. Circadian patterns of the development of ventricular fibrillation in patients with Brugada syndrome. Eur Heart J 1999;20:465-470
- Brugada P, Brugada J, Brugada R. The puzzle behind electrical chaos and sudden cardiac death in the structurally normal heart. Eur Heart J 1999;20:401-2
- Takenaka S, Emori T, Koyama S, Morita H, Fukushima K, Ohe Tohru. Asymptomatic form of Brugada syndrome, in press.
- Savard P, Cohen D, Lepeschkin E, Cuffin BN, Madias JE. Magnetic measurement of S-T and T-Q segment shifts in humans. Part I:
- Perez de Juan M, Cejado I, Fernadez L, Espinosa JS, Vicente T, De Toro JM. Bloqueo de rama derecha, elevacion del segmento ST y muerte subita cardiaca por asistolia.
- Kobayashi H, Ohonish S, Momosi M, Kusakabe K, Okawa T. Characteristic findings of I-123MIBG scintigraphy in patients with Brugada syndrome. Circulation ; : 152.
- Gussak I, Bjerregaard P, Antzelevitch CH, Nademanee K, Chaitman BR. ECG manifestation of Brugada syndrome: Clinical and electrophysiologic considerations. In press.
- Brugada J, Brugada R, Wang Q, Potenza D, Towbin JA, Brugada P. Unmasking of genotypic and phenotypic markers for sudden death by class Ia antiarrhythmic drugs in patients with a structurally normal heart. In preparation.
- Mehta M, Jain A.C., Meta A. Early repolarization. Clin Cardiol 1999;22:59-66
- Brugada syndrome: http://www.brugada.crtia.be/